In The Line, Adam Zivo reports on Ontario’s “safe supply” drug program running into another one of those pesky human nature problems that couldn’t possibly have been foreseen:
New research from Ontario has yielded further evidence that Canada’s “safer supply” drug programs are being widely defrauded and putting addicts’ lives at risk.
These programs claim to reduce overdoses and deaths by providing drug users with pharmaceutical alternatives to potentially tainted illicit substances. In Canada, that typically means distributing large volumes of hydromorphone, an opioid as potent as heroin, in the hope of reducing consumption of illicit fentanyl.
Addiction experts have widely reported that, based on their clinical experiences, drug users regularly trade or sell (“divert”) some (perhaps much) of their safer supply on the black market to fund the purchase of stronger substances. This has flooded some communities with hydromorphone, crashing its street price by up to 95 per cent over the past three years while spurring new addictions, especially among youth.
The federal government denies that these problems exist and has said that any evidence of harm is “anecdotal” — but two addiction experts working in a hospital in London, Ontario recently used patient data to show that the problem is indeed very real.
Dr. Sharon Koivu and Allison Mackinley (a nurse practitioner) examined the charts of 200 patients who had been referred to Victoria Hospital’s addiction medicine consultation service between January and June 2023.
The review showed that 32 per cent of patients who were not in a safer supply program had self-reported using diverted hydromorphone — the vast majority of these patients indicated that their hydromorphone came from purchasing drugs provided to someone else as part of a safer supply program.
“It was more common for them to actually specify safer supply than to say they didn’t know the source,” said Dr. Koivu in an interview. “They said things like, ‘The person in the apartment beside me goes and picks up her safer supply and when she comes back I get 20 of her pills’. It was quite specific.”
Diversion was not the only problem that was validated.
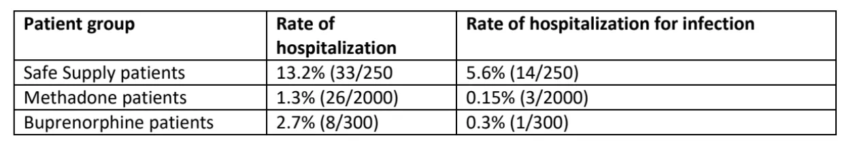
The chart data suggested that safer supply clients were roughly five-to-10 times more likely to be hospitalized than drug users receiving traditional, evidence-based addiction medications, such as methadone or buprenorphine (these medications are known as “opioid agonist therapy“, or “OAT”). Compared to OAT patients, drug users on safer supply were more than 15 times more likely to be hospitalized for serious infections.
These findings were so concerning that when a group of 35 addiction physicians recently wrote an open letter calling upon the federal government to reform safer supply, they included this data in their accompanying evidence brief.
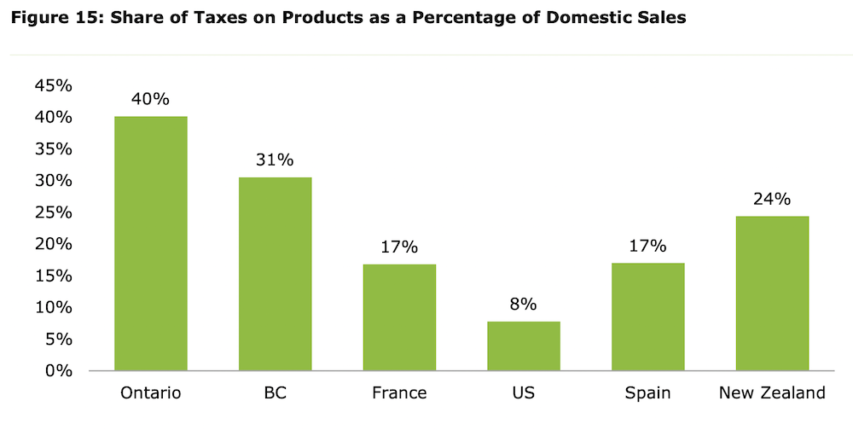
(This chart, included in a recent evidence brief, compares the number of hospitalized patients with the number of drug users in London, Ontario who receive safer supply (250), methadone (2,000), and buprenorphine (300).)
Safer supply patients also had a slightly higher hospitalization rate, and only slightly lower infection rate, than patients who were receiving no addiction treatment at all, which suggests that the health benefits of safer supply may actually be negligible.
Dr. Koivu said that the hospitalization rate seen among safer supply patients was “alarmingly high” considering that safer supply programs provide significant wraparound supports (i.e. access to doctors, housing and social assistance) in conjunction with free hydromorphone. Any patient who receives such supports should see substantially improved health outcomes.