When the Trump administration proposed imprisoning homeless people who don’t voluntarily go to shelters, and the predictable howls of outrage arose, I remembered the most interesting fact I’ve ever learned about imprisonment rates.
The US is often pilloried for having a high level of imprisonment per capita relative to other countries. The US is also quite unusual in having shut down most of its insane asylums many decades ago.
My perspective on these facts changed a great deal when I learned that if you aggregate rates of imprisonment with rates of commitment to mental institutions, the US stops looking like an outlier.
The low-level mentally ill didn’t go away when we closed the asylums. Nor did they magically become more able to function in society when we pushed them out the doors. Instead, they now land in our prisons.
Another implication of all this is that it’s not “structural racism” or any other specific evil that gives the US high imprisonment rates. It’s an inevitable consequence of the social decision to make it very difficult to involuntarily commit people to asylums.
I’m not going to argue today about whether that decision should be reversed. I have an opinion about that, but this post is about facts and consequences, not value claims or what “should” be.
Let’s return to the homeless. It is now common knowledge that homeless people are almost never simply poor or down on their luck. Almost all have serious issues with mental illness or drug addiction, or both. Many refuse to go to shelters because they don’t want to — or are not capable of — complying with a homeless shelter’s behavioral restrictions.
While I don’t have firsthand knowledge or controlled studies to back me up, it seems obvious that the shelters are acting as a filter — the least damaged and most functional homeless go to them, leaving the crazies to inhabit the streets.
Thus, throwing homeless people who won’t go to shelters in prison is an exact functional equivalent of involuntary commitment to a mental asylum.
My question for people who object to imprisoning the mentally ill and drug-addicted homeless is: what do you propose we do instead? Are we prepared to reopen the asylums and lower the bar for involuntary commitment?
I don’t think there’s a third alternative anymore. Donald Trump, whatever his other failings might be, has an acute sense of the zeitgeist; popular tolerance for having the streets of our cities inhabited by crazy people is collapsing. It turns out we can only tolerate so many news stories about naked screaming nut-jobs on the subway.
I’m not going to propose an answer to the question I just raised, because I’m conflicted about it myself. My goal is to start people thinking about the right question, which is a very large one.
What is the humane way to treat people who are too damaged or broken to be functional members of society, and who inflict large costs on others if they’re not separated from society?
If it’s not prisons or asylums, what are we going to do? And given how ineffective psychiatric treatment is at anything beyond management of symptoms, is “prison” vs. “asylum” even a meaningful distinction?
ESR, The social media site formerly known as Twitter, 2025-08-13.
November 29, 2025
QotD: Are there no prisons? Are there no asylums?
April 20, 2025
The essence of (most) modern western governments
Chris Bray on the paradox of how many western governments manage the alchemy of being both omnipresent and yet absent simultaneously:
Adding to my last post about covering language that masks the massive expansion of government behind performative language about limiting government: The most Los Angeles thing I have ever seen happened behind the Yoshinoya Beef Bowl.
See the alley between the Yoshinoya and the pharmacy? As I drove by on Wilshire, two extremely alert LAPD officers on motorcycles were sitting at the edge of that parking lot, postures tight and poised for action, urgently scanning the street. It was like watching a gunfighter movie, in the scene when the camera closes in on the gunfighter’s eyes, watching his opponent for the draw. These dudes were ready. If you did 38 in the 30 MPH zone, then brother, you were dead-ass done, nailed up in the trophy case.
Also, no more than thirty feet away from them, a little gaggle of filthy human zombies was passing a glass pipe around the circle, throwing up clouds of smoke, at the top end of an alley wall-to-wall full of open drug use and not terribly subtle drug dealing (and probably the prostitution that pays for the drugs, but I didn’t wander into the alley to look). But California made the possession and use of heroin, meth, and cocaine a misdemeanor, and the DA at the time was very proud that he wouldn’t allow his office to file most misdemeanor cases, because misdemeanors are lifestyle crimes that punish people for being poor, or for being “individuals experiencing homelessness”. So that alley full of people Hunter Bidening all day out in the open weren’t doing anything that could lead to prosecution, but your expired registration tags would bring down an immediate police response in you happened to roll by them.
Grand Guignol human depravity and ruin: no big deal. Minor traffic offenses: front and center.
This is Blue Zone governance, full stop, the thing people describe as anarcho-tyranny. Common San Francisco business owner experience: Police don’t intervene in the constant vandalism and tagging that degrades business property, but the highly alert army of code enforcement officers fine business owners for failing to clean up the damage that the city hasn’t prevented.
I forget who recently suggested this on I-still-call-it-Twitter, but go to Yelp and read some reviews for gas stations in Oakland:
January 19, 2025
California’s wildfire plight
Theophilus Chilton on the end of California dreamin’:
Southern California has had a REALLY rough week. Wildfires, started by arsonists and driven by the Santa Ana winds, have burned thousands of acres in the city and county of Los Angeles and destroyed over $150 billion worth of property (and counting). As I write this, the fires still burn and largely remain uncontained, even as new blazes break out. It is a disaster of epic proportions, striking one of the richest and most economically and culturally relevant portions of the country.
Never ones to let a crisis go to waste, the Left responded to this disaster by … focusing on climate change. Not empty fire hydrants, not drained reservoirs, not incompetent leadership, but climate change. These fires, we have been breathlessly assured, are the result of ever-worsening climatic conditions in the region, drying it out and making it susceptible to this kind of affliction. Never mind that observers since Spanish times consistently noted the same kind of weather conditions and hazards that we see today, which suggests that maybe things aren’t actually changing all that much. Of course, those who are blaming climate change fail to recognise the fundamentally chaotic, nonlinear nature of the Earth’s biosphere and the interactions of its constituent parts, something governed by complexity (in the chaos/complexity theory sense of the term). As a result, it’s somewhat foolish to try to draw a direct, causal link between two variables (such as atmospheric CO2 content and temperature) which depend upon nonlinear interactions with hundreds of other factors. Thankfully, they don’t seem to be getting much traction with this.
So what did create the conditions that burned down Los Angeles?
First of all, there was the implementation of a number of policies driven by the state’s radical environmentalist lobby. Thanks to the fanatics, common sense policies that would help to mitigate the region’s inherent fire hazard went undone. Regular controlled burns of underbrush are a standard conservation technique in dry areas that help to thin out brush and prevent wildfires from getting out of control. Building a sufficient number of desalination plants is a good way for coastal desert areas to provide themselves with abundant fresh water for things like drinking, watering crops, filling reservoirs, and fighting fires. In fact, filling reservoirs for future needs would make a lot of sense. But all of these things are “unnatural” and might have “negative impacts” on local wildlife and whatnot.
Another contributory issue is the state’s policies towards the chronically homeless and its de facto sanctuary status for illegal aliens. The Reagan-era deinstitutionalisation of the homeless has been a nationwide disaster for years and California’s particular policies have made the situation in their state even worse. For decades, California has regularly seen wildfires caused by untended campfires started by homeless junkies getting out of control, which the state’s liberal approach to its indigent population has only made more prevalent. Likewise, California’s harbouring of illegal aliens has created a situation in which the state is flooded with masses of hostile foreign elements, some of whom have been caught starting fires all around the LA basin and creating the current catastrophe.
Then there is the fact that California has systematically implemented a set of DEI policies for its governmental workers, including its firefighters. As a result, the state’s leadership in the relevant departments is very good at “promoting inclusion,” but not so good at dealing competently with emergencies when they take place. Indeed, Los Angeles’ mayor Karen Bass and LAFD Chief Kristen Crowley presided over budget cuts for the city’s firefighting capabilities while adding layers of “diversity and inclusion” bureaucracy aimed at systematically de-white-maleing the department and depriving it of the demographic most prone to self-sacrifice and overall technical competence. That reflects trends across the board in which the state and the city have regularly spent more on gay choirs and social justice artwork than they have on necessary functions of government.
October 6, 2022
The pendulum swings back toward institutionalization
During the 1950s and 60s, many mental institutions were shut down due to concerns about the way the patients in those institutions were being treated. Those suffering from mental health issues were, to a large degree, just discharged into the larger community with few supports to help them re-integrate. Today, the concerns about severely mentally ill peoples’ actions may be pushing the system back toward some form of formal re-institutionalization, as Michael Shellenberger reports for Common Sense:
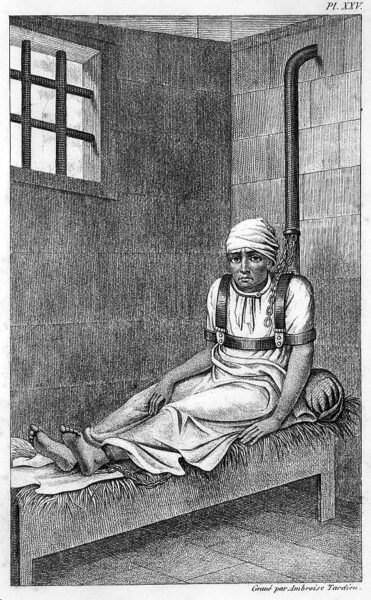
William Norris, shackled sitting upright on his bed at Bedlam, 1838.
Engraving by Ambroise Tardieu, Des maladies mentales Esquirol via Wikimedia Commons.
Though it is difficult to get an exact estimate, a large body of research makes clear that people like Zisopoulos, Mesa, and Simon are just three among hundreds of cases of people in New York alone — to say nothing of cities like Los Angeles, Seattle, San Francisco and others — in which mentally ill people off their medication have assaulted or killed people. And if you think the problem is getting worse, you are right.
In 2021, felony assaults in New York’s subway were almost 25 percent higher compared to 2019, despite a lower ridership because of the pandemic. The number of people pushed onto tracks rose from 9 in 2017 to 20 in 2019 to 30 in 2021. Psychiatrists and emergency department workers in San Francisco and Los Angeles tell me that they have seen a significant increase in homeless patients in psychotic states over the last few years.
How have we arrived at the point where we leave people with psychosis to their demons, and leave the public to take their chances? How have we allowed so many of our cities to have no decent plans or places for the burgeoning number of the violent mentally ill on the streets?
There are two major forces at work. The first is that the U.S. never created a functioning mental health care system. The second is that powerful groups have effectively prevented dangerously mentally ill people from getting treatment.
Starting in the late 19th century, the U.S. created large psychiatric hospitals, often in the countryside, known as asylums, for the mentally ill. Asylums were a major progressive achievement because they delivered, for many decades, significantly more humane, evidence-based care to people who, until then, had often been neglected, abused, or even killed.
But by the middle of the 20th century, the reputation of psychiatric hospitals was in tatters — and deservedly so. Conditions in many of them were appalling, even barbaric. People who were not severely mentally ill were sometimes subjected to years of involuntary hospitalization.
Many reformers just wanted better funding and oversight, but other reformers were more radical, and proposed shutting the hospitals down entirely and replacing them with community-based clinics. Some reformers claimed that serious mental illnesses were the result of poverty and inequality, not biology, and argued that they could be cured through radical social change.
The reformers largely won. State hospitals were shut down in droves before sufficient community centers could be built to treat the suffering. Over the next two decades, as state mental hospitals emptied out, many released patients ended up on the street, or incarcerated. Those community clinics that did start operating tended to treat “the worried well” — those suffering from comparatively low-level anxiety and depression, rather than psychosis.
Decades later, governments were still cutting funding for the treatment of the mentally ill. New York State in 2010 reduced Medicaid reimbursement for inpatient stays of the mentally ill in hospitals beyond 12 days. As a result, New York hospitals released the mentally ill earlier than they should have. From 2012 to 2019, the number of mentally ill adults in inpatient psychiatric care in hospitals and mental institutions in New York City declined from 4,100 to just 3,000. Meanwhile, the number of seriously mentally ill homeless people rose from 11,500 to 13,200.
The story is similar in California. Between 2012 and 2019, more than one-third of the group homes in San Francisco that served mentally ill and disabled people under the age of sixty closed their doors. Why? The measly Medi-Cal and Medicare reimbursement of $1,058 per person per month, and rising estate prices, made it more valuable for the private owners of group homes to sell than to keep operating them.
At the national level, the same dynamic was in play. The U.S. as a whole lost 15,000 board and care beds for the mentally ill and disabled between 2010 and 2016. Today, approximately 121,000 mentally ill people are conservatively estimated to be living on America’s streets.
September 22, 2022
California’s Central Valley of despair
At Astral Codex Ten, Scott Alexander wonders why California’s Central Valley is in such terrible shape — far worse than you’d expect even if the rest of California is looking a bit curdled:
Here’s a topographic map of California (source):
You might notice it has a big valley in the center. This is called “The Central Valley”. Sometimes it also gets called the San Joaquin Valley in the south, or the the Sacramento Valley in the north.
The Central Valley is mostly farms — a little piece of the Midwest in the middle of California. If the Midwest is flyover country, the Central Valley is drive-through country, with most Californians experiencing it only on their way between LA and SF.
Most, myself included, drive through as fast as possible. With a few provisional exceptions — Sacramento, Davis, some areas further north — the Central Valley is terrible. It’s not just the temperatures, which can reach 110°F (43°C) in the summer. Or the air pollution, which by all accounts is at crisis level. Or the smell, which I assume is fertilizer or cattle-related. It’s the cities and people and the whole situation. A short drive through is enough to notice poverty, decay, and homeless camps worse even than the rest of California.
But I didn’t realize how bad it was until reading this piece on the San Joaquin River. It claims that if the Central Valley were its own state, it would be the poorest in America, even worse than Mississippi.
This was kind of shocking. I always think of Mississippi as bad because of a history of racial violence, racial segregation, and getting burned down during the Civil War. But the Central Valley has none of those things, plus it has extremely fertile farmland, plus it’s in one of the richest states of the country and should at least get good subsidies and infrastructure. How did it get so bad?
First of all, is this claim true?
I can’t find official per capita income statistics for the Central Valley, separate from the rest of California, but you can find all the individual counties here. When you look at the ones in the Central Valley, you get a median per capita income of $21,729 (this is binned by counties, which might confuse things, but by good luck there are as many people in counties above the median-income county as below it, so probably not by very much). This is indeed lower than Mississippi’s per capita income of $25,444, although if you look by household or family income, the Central Valley does better again.
Of large Central Valley cities, Sacramento has a median income of $33,565 (but it’s the state capital, which inflates it with politicians and lobbyists), Fresno of $25,738, and Bakersfield of $30,144. Compare to Mississippi, where the state capital of Jackson has $23,714, and numbers 2 and 3 cities Gulfport and Southhaven have $25,074 and $34,237. Overall Missisippi comes out worse here, and none of these seem horrible compared to eg Phoenix with $31,821. Given these numbers (from Google), urban salaries in the Central Valley don’t seem so bad. But when instead I look directly at this list of 280 US metropolitan areas by per capita income, numbers are much lower. Bakersfield at $15,760 is 260th/280, Fresno is 267th, and only Sacramento does okay at 22nd. Mississippi cities come in at 146, 202, and 251. Maybe the difference is because Google’s data is city proper and the list is metro area?
Still, it seems fair to say that the Central Valley is at least somewhat in the same league as Mississippi, even though exactly who outscores whom is inconsistent.
November 4, 2021
June 8, 2021
If you were trying to destroy American cities from within … what would you be doing differently?
Sarah Hoyt’s latest Libertarian Enterprise post considers the state of US urban areas after more than a year of Wuhan Coronavirus lockdowns, social controls, and medically “justified” repression:

“Homeless encampment above the 101 @ Spring” by Steve Devol is licensed under CC BY-NC-SA 2.0
Look, I’m sure this was suggested by China, and the dunderheads are totally buying it under their Compleate Illusions system.
Sure climate change. Climate change can justify anything. If we told them they needed to burn people alive to prevent climate change, they’d already been building the pyres.
But that’s just sort of a reflexive thing, like a Moslem saying “Insh Allah“. It’s not actually involved in their thinking as such. Or their thinking is not involved in it. whichever.
The truth is that they realized that the Covidiocy has destroyed the cities.
You see they had everything planned. They were going to force more and more of us into the city, because they were going to make running an internal combustion engine so hard. So if you had a job, you’d live in the city. Where you’re more easily controlled. And where they could make you believe bullshit like overpopulation and that — look at all the homeless — we needed more and more welfare. Their idea of their perfect world is the 1930s version of the future. Just megalopolisis, isolated, with people completely controlled. It has the bonus of leaving pristine wilderness outside that, for the elites to build their dachas.
And part of the problem is that they never understand other people have agency and respond to circumstances.
I don’t know what they expected when they went full fashboots and — in the case of Polis, and I bet not the only one — gave homeless the right to camp in every public land, and defecate in public as well as freeing a bunch of felons.
Did they expect this would just scare people more, and they’d lock themselves in, in fear and trembling, allowing the idiots to design society.
Instead, people left. Americans are on the move. I swear half of my friends are moving from more locked to less locked, from bluer to redder. Some demographers have caught on, seeing through the smoke and mirrors, and are confused — most of them being leftist — because Americans are in the middle of a full migration. As full and as all pervading as the movement west. Or after the civil war the movement of black people North.
Some of this must have penetrated the granite-like heads of the ruling left. Or at least the planning left.
They somehow didn’t expect—possibly because they don’t really get technology. I mean, I have my moments, but I swear most democrats were disappointed when laptops started being made with no “cup holders”. They’re at that level of stupid — that a tech that hasn’t been fully implemented, giving us the ability to work from home, would be kicked into high gear from the covidiocy.
I guess they expected people who work mostly from their computers to sit at home watching panic porn on TV and not work?
More importantly, I don’t think they expected people who have to work in person to follow that migration because, well … if you owned a restaurant that the covidiocy killed, you might, for instance, pay heed to the fact people are driving everywhere because, duh, masks on planes, and therefore build a roadside diner or perhaps find a small town that’s underserved and start anew there.
Oh … a lot of people are changing jobs too, and the jobs are no longer binding them to big cities.
Honestly, the only way for big cities to save themselves is to become touristic centers. NYC was halfway there when the covidiocy hit. Only not fully there because lefty governance sucks at making a city safe.
If I were a lefty governor or mayor right now, I’d aim the fashboots at crime and disorder, get rid of the homeless, spruce up the place, and go all out in courting tourism. Then people would move in to cater to the tourists, and eventually other businesses would move in, because that’s where people are.
But leftists don’t think that way. Carrot and incentive is beneath them (of course.) Their idea is rather that they will force those unwashed peasants to do what they want.
April 5, 2021
QotD: NYC goes out of its way to “afflict the comfortable”
In July, the city moved 700 homeless single men into hotels on the densely populated and famously tolerant Upper West Side, purportedly as a response to the pandemic. Residents were stunned to find their neighborhood turned overnight into a skid row, with nonstop open drug sales and drug use, public sex acts, and rampant street harassment of women and girls. During a contentious local community board Zoom meeting about the issue, Erin Drinkwater, a deputy commissioner of intergovernmental and legislative affairs at the Department of Social Services, spoke blandly about the need for “compassion” and implied that the concerned neighbors were racist for opposing the city’s move. Following the meeting, Drinkwater tweeted “Comfort the afflicted; afflict the comfortable.” When asked what she meant by this, she said that it was a quotation from the Bible’s Book of James, and that it spoke to her sense of mission.
One might ask why a social-services functionary in New York City would cite the Bible in defense of public policy — except that the quotation is not even from the Bible. In fact, it is from Finley Peter Dunne, a popular Chicago columnist from the 1890s who invented a humorous character named “Mr. Dooley,” an Irish bartender who delivered his wisdom in dialect.
The original quotation, in which Mr. Dooley described the function of the newspaper: “Th’ newspaper does ivrything f’r us. It runs th’ polis foorce an’ th’ banks, commands th’ milishy, controls th’ ligislachure, baptizes th’ young, marries th’ foolish, comforts th’ afflicted, afflicts th’ comfortable, buries th’ dead an’ roasts thim aftherward.” Somehow, in a bizarre game of “cultural telephone,” this mock-sonorous fiddle-faddle has gathered the effulgence of holy writ for progressives, who take it as descriptive of their “joyous responsibility.”
On the one hand, it’s comical that this scrap of tabloid wit is taken so gravely by self-righteous officials. Properly speaking, isn’t it their job to make people more comfortable, not to diminish comfort? But on the other hand, it’s frightening to consider that New York is now run by progressive militants who appear to believe that their vocation is to “afflict” their constituents by disrupting their undeserved calm and comfort. Mass immiseration is not a side effect of bad policy; it is the policy.
Seth Barron, “The Politics of Affliction”, City Journal, 2020-12-17.
January 20, 2021
QotD: Helping the homeless
I understand that the general media explanation of homelessness is to blame it on the cold heart of whoever was the last Republican President in office, but it is hard for me to correlate national policy with trends in homelessness. I am maybe 70% convinced that the closing of mental health facilities in the 70’s and 80’s across most cities and states was the main cause, a hypothesis born out by the high rates of mental illness recorded in most homeless populations. This is why I think so much government spending for the homeless is wasted — it all focuses on creating homes, I guess just because of our word choice of “homeless”. If we called them the mentally ill, or perhaps “helpless” rather than “homeless” we might investigate other approaches.
I see a number of sources nowadays trying to pin these closures entirely on tight-fisted Republican governors, and I am sure this is partly true. But this misses an important element — that civil libertarians had real issues with both the conduct of these institutions (e.g. One Flew Over The Cuckoo’s Nest) and the fairness of the forced-institutionalization process. Also tied up in all this were Cold War stories of Soviet Russia using institutionalization in mental hospitals as a way to dispose of dissidents. After all, it is a short step from the totalitarian view of ideology (ie that everyone must believe, not just comply) to declaring that any deviation from the official orthodoxy constitutes mental illness.
Warren Meyer, “Why I Go Back and Forth On Issues of Forced Psychiatric Institutionalization”, Coyote Blog, 2018-09-20.
September 27, 2020
Homelessness in Los Angeles
In Quillette, Amy Alkon talks about the homeless crisis in LA, particularly her own immediate experience with a couple who “camped out” in front of her house.
Throughout [Los Angeles Mayor Eric] Garcetti’s seven years as Mayor, Los Angeles has witnessed a shocking explosion of homelessness. When he took office in 2013, the city had about 23,000 residents classified as homeless, two thirds of whom were unsheltered, living on the streets. By mid-2019, the figure was about 36,000, and three-quarters of them were living on the streets. Currently, there are 41,000 homeless. Garcetti’s pet plan to alleviate the homelessness crisis was the construction of permanent supportive housing. In 2016, compassionate voters approved $1.2 billion in new spending to fund these units. Three years later, only 72 apartments had been built, at a cost of about $690,000 apiece. Meanwhile, an El Salvador-based company has come up with nifty $4,000 3D-printed houses that look like great places to live and can be put up in a single day.
There’s also been a failure to admit that housing alone isn’t the solution. As urban-policy researcher Christopher Rufo explains, only about 20 percent of the homeless population are people down on their luck, who just need housing and a few supportive services to get back on their feet. Approximately 75 percent of the unsheltered homeless have substance-abuse disorders and 78 percent have mental-health disorders. Many have both.
As a bleeding-heart libertarian, I feel personally compelled to try to help people who are struggling. I do this by volunteering as a mediator, doing free dispute resolution to provide “access to justice” to people who can’t afford court. And since about 2009, I personally have given support to one of those easily helpable 20 percent Rufo refers to, getting him paying work and a bank account, and storing his stuff in my garage. He is a good man and a hard worker — sober for many years — who simply seems to have issues in the “front-office” organizational parts of his brain that help most of us get our act together to, say, pay bills on time. He just needs somebody to back him up on the bureaucratic aspects of life. I’m happy to say he now has a roof over his head. He lives in a motel across the country, and all I still do for him is provide him with a permanent address. I receive his Veterans Administration and Social Security mail at my house, which I mail to him with smiley faces and hearts on the envelopes, colored in with pink and orange highlighter.
This success story would not be possible for most homeless people, the nearly 80 percent who are addicted and/or mentally ill. As Rufo writes:
Progressives have rallied around the slogan “Housing First,” but haven’t confronted the deeper question: And then what? It’s important to understand that, even on Skid Row, approximately 70 percent of the poor, addicted, disabled, and mentally ill residents are already housed in the neighborhood’s dense network of permanent supportive-housing units, nonprofit developments, emergency shelters, Section 8 apartments, and single room-occupancy hotels.
When I toured the area with Richard Copley, a former homeless addict who now works security at the Midnight Mission, he explained that when he was in the depths of his methamphetamine addiction, he had a hotel room but chose to spend the night in his tent on the streets to be “closer to the action.” Copley now lives … at the Ward Hotel — which he calls the “mental ward” — where he says there are frequent fights and drugs are available at all hours of the day. The truth is that homelessness is not primarily a housing problem but a human one. Mayors, developers, and service providers want to cut ribbons in front of new residential towers, but the real challenge is not just to build new apartment units but to rebuild the human beings who live inside them.
The situation is especially tragic for those who are so mentally ill that they cannot take care of themselves, and are often a danger to both themselves and others. And I sometimes wonder which movie star or other famous person needs to be stabbed or bludgeoned before politicians take meaningful action.
It’s fashionable in progressive circles to demonize law enforcement, but Rufo explains that in 2006, then-L.A. police chief Bill Bratton implemented a “Broken Windows” policing initiative on Skid Row. It led to a 42 percent reduction in felonies, a 50 percent reduction in deaths by overdose, and a 75 percent reduction in homicides. The overall homeless population was reduced from 1,876 people to 700 — a huge success. Activists filed lawsuits and ran publicity campaigns, slowly killing Bratton’s program, on the grounds that it “criminalizes homelessness.” As a libertarian, I’m opposed to drug laws and forced behavior — but only to a point. It is not compassion to leave people to be victimized by criminals simply because they are unhoused, nor is leaving mentally and physically disabled people strewn across the streets amidst piles of garbage a form of freedom.
Mayor Garcetti, in lieu of admitting the real challenges — the first step to taking meaningful action to alleviate the homelessness crisis — has simply ignored the human results of his failed policy. As a result, whole sections of the city, including formerly livable streets in my beloved Venice, have been turned into Skid Row by the Sea.
September 15, 2020
When you mix up cause and effect
In the Continental Telegraph, Esteban remembers a Reagan bon mot that is still observably true today:

US President Ronald Reagan and Soviet General Secretary Mikhail Gorbachev at the Hofdi House in Reykjavik, Iceland during the Reyjavik Summit in 1986.
Official US government photograph via Wikimedia Commons.
Ronald Reagan once observed that “the trouble with our liberal friends isn’t that they are ignorant, it’s that so much they know isn’t so”. I am repeatedly surprised by Leftists’ ability not to just get something wrong, but to get it spectacularly, 180 degrees wrong.
First, a couple of examples from the archives – some years ago there was an article in the NY Times (or WaPo perhaps) quite distressed that even though crime rates in the U.S. were at historically low levels the percentage of the population in prison was quite high. “Why are we putting so many people in prison when the crime rate is low?” they wondered, seriously. Hmm, how about this – when we put more bad people in prison the crime rate goes down? Keep in mind that the crime rate is what’s happening now, the prison population is who we caught and locked up over the past several years.
Then we had an article in a West Coast newspaper wondering why the homeless population in San Francisco had grown dramatically in recent years despite all the wonderful things the city had done to help them – weekly stipends, free shopping carts, etc. Note that none of this assistance to the homeless enabled them to become independent or required them to better themselves, they were all handouts. How is it that offering lots of goodies to homeless people attracts more of them here?
My point in bringing up these old stories is that it seems impossible that someone could fail to see they had cause and effect reversed. How could someone intelligent enough to write a column get these stories so backwards. The only answer I can see is that their worldview, at least in these areas, flows in only one direction and the underlying premise can never be questioned – putting people in prison is bad, there can be no possible upside, giving homeless people stuff is good, there can be no downside. So, when things get worse it’s a mystery, we can’t reconsider our starting point.
June 12, 2020
QotD: Homelessness in America
First let’s start with the fact that homelessness as it exists in America isn’t poverty. In fact part of the problem with it is that it ISN’T poverty. Look, regardless of what you’ve seen on the movies or TV, most homeless are not families fallen on hard times. Yes, there are some of those now, but most of those while technically “homeless” aren’t living in your local park. They’ve just taken over mom and dad’s basement, moved onto a friend’s living room or whatever. Terrible – I’ve been JUST short of that at least three times in my married life – and humiliating, but NOT “stand in the park and wheedle on yourself.”
90% of the homeless in America and the hard core ones are people with mental health issues, people with drug abuse issues and people who have found they can live without having to do anything for it, and can be “free” and outside society. I’ve overheard conversations in the park, and I suppose that most of the people who “dropped out” in the sixties are dead, but a lot of them are alive and going from soup kitchen to free clinic, with a bit of begging in between.
Yes, there are entire families in this system, including homeless children – but for them to stay in it, the parents need to have some sort of serious issue. Otherwise, even if they can’t find work, there is assistance available to get them at least into public housing, which, nightmarish though it is, is not living in the park.
I’m not going to pretend this doesn’t happen to normal families too – see where I came very close to that level and more than once too – but normal families usually tend to bounce back. They go through a few months of mess and horror, and then they claw back to some semblance of normalcy. (This might change as our economy dives and programs of necessity get cut. The ones for the DESERVING poor will be cut first, of course, since they rarely riot.)
The problem with this is that when people get appalled at the conditions the homeless live in and start offering “homeless services” there is an entire network, not just of homeless but of social workers who direct the homeless to the cities with better services.
I swear to you and I’m not even joking that right now there are plenty more homeless on Colorado Springs streets than in Denver, despite the Springs being much smaller.
The Springs also has its soup kitchens and other services downtown and within easy walking distance of each other.
This means downtown businesses are closing, except for bars and restaurants which can control access. And that the library is of course a place to camp in the cool/warm during the day.
It means more than that. We moved within easy driving distance of downtown, because when we lived downtown when we first came to Colorado Springs, I used to take walks every day. When we moved to our little mountain village, without these, I gained ten pounds a year. I used to love walking downtown, dropping by the deli and the three bookstores (only one left, and it’s MOSTLY a restaurant now) checking out the other little shops which ranged from yarn to weird import crafts.
Now those are gone. Worse – the last two times I walked downtown alone (i.e. without commanding the muscle, aka older son to go with me) someone FOLLOWED me and I had to employ stuff from my childhood to lose them. Once it was a large and addled looking male, and yes, he was following me. And once it was TWO large and addled looking males. For the icing on the cake – not related to this, but from a blog entry – I clicked on the sex offenders registry. Yes, I know, a lot of people there are there because someone accused them and was never proven. Our local one at least has notes on whether it’s accusation, trial or conviction and also whether the crime was against children or adults.
The downtown zipcode is FULL of registered sex offenders who’ve done hard time and who have committed their crimes against adults. The faces are very familiar from my walks, and yep, one was the guy who tried to follow me.
Sarah Hoyt, “Of Books, Compassion And Cruelty A Blast From The Past From June 2013”, According to Hoyt, 2020-03-10.
May 10, 2020
London’s Metropolitan Police live down to expectations … and then some
Brendan O’Neill observes the latest sweep by the Metropolitan Police, relentlessly cracking down on scofflaws and evil-doers who … were walking peacefully in the sunshine?

Armed Metropolitan Police near Downing Street in London.
Photo by Stanislav Kozlovskiy via Wikimedia Commons.
You heard them before you saw them. It sounded like a platoon of soldiers. The one in charge was barking orders to “move forward!” and then came the trudge of their boots. Scores of them, making military manoeuvres, marching in a long, thin line through one of Britain’s prettiest parks: St James’s Park in London. This was the Metropolitan Police today, enforcing the lockdown, sweeping through parks and streets and issuing the same warning to everyone they came across, from young lovers to dads playing football with their kids to homeless people with nowhere else to go: “Move on.” It’s one of the most disturbing things I’ve ever seen the police do.
Watching them stream through St James’s Park, looking for all the world like a line of soldiers conquering a small town, you’d think they were on their way to confront some serious organised crime. But of course their targets were sunbathers, those apparently selfish people demeaned in the media and now harassed by the cops. And a dad playing football with his toddler. “Aren’t we allowed to exercise?”, the dad asked. “For one hour”, came the reply. “How long have you been out?” And young lovers and friends. I saw a copper on horseback shouting down at two young men as if they were in the process of committing some awful crime. I guess they were in the eyes of the lockdown fanatics: they were sitting under a tree.
A young Muslim mum sitting down and watching her two kids play with little tennis bats was confused, too. Can’t kids play outside? She was told she couldn’t sit still. She had to walk. “How about walking your kids around the park?”, said the spectacularly patronising cop. They even threw out homeless people. I saw them tell four individual homeless people (ie, not a group of homeless people) to move on. Where to? Must they also walk and walk, forever, and never sit down anywhere? The most despicable thing I saw was a policeman telling an elderly homeless gentleman to move on. Inarticulately, the man explained he had nowhere else to go. I stepped in and explained to the cop that there is no home for him to go to, and he has to be able to sit down somewhere on a hot day. “I don’t make the rules”, came the snivelling, officious reply.
The police’s reputation will have taken a severe beating in London today. Anyone who argued back — as two young women did, patiently explaining that they are from the same household and that they were metres away from everyone else — was patronised or even insulted. “You’re putting other people’s lives at risk”, the women were told, which is completely untrue — being outside and socially distanced on a very warm day carries virtually zero threat of infection. I heard an officer call someone an idiot. Another officer made fun of someone who asked about his right to be outside. It was staggeringly rude and even repugnant behaviour. A politician, or someone, needs to get a grip on these people.
March 15, 2020
Those damned unintended consequences
Sarah Hoyt on the differences between intention and the real world:
Unintended consequences are the bane of social engineers. They are why the “Scientific” and centralized method of governance never worked and will never work. (Sorry, guys, it just won’t.)
Part of it is because humans are contrary. Part of is because humans are chaotic. And part of it is because like weather systems, societies are so complex it’s almost impossible to figure out what a push in any given place will cause to happen in another place.
This is why price controls are the craziest of idiocies. They don’t work in the way they’re intended, but oh, they work in practically all the ways they’re not. So, take price controls on rent. All they really do is create a market in which housing is scarce, landlords don’t maintain their property AND the only people who can afford to live in cities that have rent control are the very wealthy.
BUT Sarah, you say, aren’t rent controls supposed to make them affordable. Yeah. All that and the good intentions will allow you to go skating in hell on the fourth of July weekend.
Let’s be real, okay? I saw rent control up close and personal in Portugal. Rents were controlled and landlords were penalized for “not keeping the property up”.
In Portugal at the time, and here too, most of the time from what I’ve seen, the administration of property might be some management company, but that’s not who OWNS the damn thing. The owners are usually people who bought the property so it would support them in old age/lean times.
To begin with, you’re removing these people’s ability to make money off their legitimately owned property. And no, they’re not the plutocrats bernie bros imagine. These are often people just making it by.
Second, people are going to get the money some other way, because the alternative is dying. And people don’t want to die or be destitute. So they’re going to find the money. I have no idea what it is in NYC, etc, but in Portugal? it was “key buying.” Sure, you can rent the house for the controlled price, but you have to make a huge payment upfront to “buy the key.” From what I remember this was on the order of a small house down payment. And if you couldn’t do that, you were stuck getting married and living with your parents. And if you say “greedy landlords” — well, see the other thing you could do was leave the lease in your will. So the landlord didn’t know if they’d ever get control of their property back, and they needed to live off this for x years (estimated length of life.) So, that was an unintended consequence. The kind that keeps surfacing in rent-controlled cities in the US.
The same applies to attempts to “help” the homeless. Part of this, as part of all attempts to “fix” poverty is that the people doing it, usually the result of generations of middle class parents and strives assume the homeless and the poor are people like them.
To an extent, they’re correct. The homeless and the poor are PEOPLE. But culture makes a difference, and culture is often based on class and place of upbringing. And the majority of humanity, judging by the world, might be made to strive but are not natural strivers. Without incentive, most of humanity sits back, relaxes and takes what it’s given.
January 6, 2016
QotD: De-institutionalization and mental health
Look, part of the whole problem with the deinstitutionalisation of the mentally ill, which goes all the way back to the early seventies at least, and as far as theory is concerned probably a lot further, is that health professionals started, DELIBERATELY blurring the lines between mental illness and mental health.
Part of this was – I think – a genuine effort to make it possible for some people classified as “mentally ill” to be able to make a go of it in the community. A lot of new psychiatric drugs had been discovered which, while they didn’t heal, masked the symptoms of mental illness and therefore made it possible for these people to integrate in normal society – provided they would take their meds (more on that later.)
The other part – I know, my SIL took the mental-health portion of her MD in the late seventies – was the insane “equivalence brigade” which tried very hard to convince themselves that the US too did EXACTLY the same things the USSR did. Since the USSR put political dissenters in mental hospitals, then the people in US hospitals MUST be also political dissenters. This was hard to prove, since the Soviet system provided ideological support for mental treatment of dissenters: i.e. the Marxist system was perfect, so anyone disagreeing must be mad, while the American system mostly tried to get people off the streets who would do harm to themselves and/or others. However the medical profession found their justification in an upside-down of the Marxist system. Since Capitalism was bad for humans and other living things, then everyone who went mad under capitalism were, ipso facto, political dissenters. So, if you happened to be a woman who liked to throw rocks at strangers and go into bizarre monologues on the subject of cabbage, you weren’t mad, you were a feminist protesting male aggression.
Now I have no proof this was intentional or a coordinated AGITPROP operation. It’s entirely possible it was (merely) the predictable mix of ill-intentioned agents and well-intentioned idiot fellow travelers.
However the end result was making people too crazy to live alone into political victims and incidentally to give the USSR room to claim the capitalist system created homelessness.
Sarah A. Hoyt, “I’m Not Crazy, I’m Just A Little Unwell – A blast from the past post 10/12”, According to Hoyt, 2015-10-12.